Document disorder stalls injury claims; amaise AI sorts files in seconds, surfaces insight, and lets adjusters focus on their expertise.
%20(1).png)
Auto-liability carriers sit at the intersection of rising accident frequency, social inflation, and an aging workforce. In the United States, the average auto-liability claim for bodily injury reached approximately $26,501 in 2023, more than four times the average of $6,551 for property-damage claims.
Bodily injury (BI) cases make up a relatively small portion of motor-vehicle claims, yet they consume a disproportionate share of indemnity costs. Motor-vehicle collisions remain the leading cause of personal-injury claims, and legal changes, higher life expectancy, and growing claims awareness continue to drive costs upward. At the same time, heavy caseloads, fragmented information, and regulatory complexity are straining claims departments.
This blog outlines the unique pain points faced by mid-size and large auto-liability carriers, then explains how amaise’s agenticAI Platform solves them with a purpose-built combination of
document organization, conversational AI, and expert-level analytics.
Key Takeaways
- Bodily injury claims drive disproportionate costs: Average injury claims (~$26,501) are more than four times the average property-damage claim and account for a small share of cases, yet they comprise the majority of indemnity costs.
- Operational strain is increasing: Rising accident frequency, social inflation, and staff shortages create heavy caseloads and fragmented workflows, making timely triage and reserve accuracy difficult.
- Agentic AI delivers a measurable ROI: amaise’s agenticAI Platform organizes documents, surfaces actionable insights, and drives a reduction of approximately 10% in claim payouts while boosting adjuster productivity by 84%.
Operational Headwinds in Auto‑Liability Injury Claims
Document Chaos and Evidence Drag
Adjusters must gather police reports, medical bills, lien statements, witness statements, telematics data, and, in some cases, body-camera footage. These documents arrive piecemeal and often in unstructured PDF format. Mid-size BI adjusters routinely handle 100–150 active claims, while large carriers handle 125–180; at such volumes, adjusters have less than 30 minutes per week for deep work. Chasing documents and re-keying data across multiple systems consumes valuable time, increases the risk of errors, and leads to a backlog of diary entries.
Early Attorney Involvement and Nuclear Verdict Risk
Over a third of claimants retain legal counsel within the first week of filing a claim. Plaintiff attorneys send 30-day “limit demand” letters that force carriers to either pay policy limits or risk bad-faith litigation. This dynamic is exacerbated by social inflation; jury awards exceeding $10 million have become commonplace, making early triage and reserve accuracy critical. Major-case adjusters worry that a misread on a single file could result in a $20 million-plus verdict and board-level scrutiny.
Caseload Overload and Talent Shortages
Claims teams are understaffed at both mid-size and large carriers. Supervisors often oversee 500–1,200 open claims, handle 50 or more payment/reserve approvals each week, and coach new adjusters while backfilling vacated positions. The retirement of 25-year veterans leaves knowledge gaps, prolongs onboarding, and contributes to inconsistent reserving and settlement practices.
Siloed Systems and Legacy Integration
Carriers rely on a patchwork of core systems, litigation management software, billing modules, SIU tools, and medical review platforms. For large carriers, these bolt-ons have been layered over decades and rarely communicate with each other. Adjusters routinely copy and paste information across systems, increasing the likelihood of duplicate payments, missed subrogation, and compliance breaches. Mid-size carriers may operate fewer systems but face lean IT budgets and lack specialized analytics, forcing adjusters to multitask across injury, litigation, and subrogation functions.
Complex Collaboration and Compliance
Injury claims require input from adjusters, supervisors, nurse case managers, medical bill reviewers, SIU teams, defense counsel, and sometimes reinsurers. Coordinating across these stakeholders without a unified view leads to delays. Carriers must also navigate 50-state response timelines; a single overdue letter can trigger regulatory fines. Supervisors spend mornings manually checking diaries to avoid missing statutory deadlines.
Reserve Volatility and Leakage
Social inflation, medical-cost escalation, and attorney tactics cause reserve levels to fluctuate wildly. Duplicate payments, late IME requests, and missed subrogation opportunities can add $6% or more to loss costs at some carriers. For mid-size carriers, limited analytics make it challenging to identify the 5%–10% of claims driving 80% of severity. In contrast, large carriers must manage multi-state leakage at scale and justify reserves to auditors and reinsurers.
How amaise’s AgenticAI Platform Unblocks Your Workflow
amaise is an AI-powered claims intelligence platform specifically designed for injury claims. Unlike generic document-processing tools, it combines large language model (LLM) agents, knowledge graphs, and an intuitive conversational interface to deliver actionable insights.
By analyzing the full case file, not just the medical record, amaise helps carriers resolve injury claims faster, more accurately, and at lower cost.
The Auto Liability solution is built on four pillars:
1. Automatic Document Organization amaise ingests the entire claim file, police reports, medical records, legal filings, and adjuster notes and automatically organizes them into a structured, deduplicated repository. Critical documents are indexed and cross-referenced, allowing adjusters to locate key information quickly. This eliminates manual sorting and re-keying, freeing adjusters to focus on investigation and negotiation. As one adjuster noted, amaise enables them to “find specific file items at lightning speed” and link arguments directly to the corresponding documents.
2. Enhanced Insights and Analytics The platform highlights injury details, accident specifics, witness statements, and policy coverage, giving adjusters a clear view of liability and damages. AI models generate multi-perspective recommendations, including pro-insurance, pro-claimant, and neutral assessments, for liability determinations, settlement ranges, and potential legal exposure. Carriers can customize question sets and evaluation templates to ensure consistent analysis across jurisdictions and claim types. These capabilities enable adjusters to triage claims quickly, set accurate reserves, and determine whether to settle or litigate.
3. Conversational AI and Agentic Workflows amaise uses conversational interfaces so users can pose complex, claim-specific questions in plain language and receive precise answers. Behind the scenes, specialized AI agents, such as document classification agents, fraud detection agents, and medical injury agents, process unstructured data and surface valuable insights. This agentic framework allows adjusters, supervisors, and medical experts to interact with claims data as if they were chatting with a knowledgeable colleague. It also captures organizational knowledge and makes expertise accessible to new hires, addressing the looming retirement gap.
4. Built-In Compliance and Easy Integration Designed for insurance, amaise adheres to HIPAA, SOC 2, and U.S. state-regulatory requirements. Implementation is lightweight: carriers can launch a pilot by uploading 30–50 claims, and full deployment typically requires around 20 person-days. The platform overlays existing core systems, minimizing disruption and eliminating the need for expensive system replacements. This is crucial for large carriers grappling with decades of bolt-on technology.
Quantified Benefits
amaise’s Auto Liability solution delivers measurable results. The platform improves adjuster efficiency by 84%, provides a 4 times better understanding of medical and legal aspects, and achieves a 10% reduction in claim payouts. European insurers using the product have documented a 10% reduction in claim payouts, and pilot programs with major U.S. carriers have shown similar performance. For large carriers, reductions in claim payouts of up to 13% have been observed while simultaneously accelerating claims processing and cutting administrative costs. By optimizing settlement decisions and enhancing fraud detection, amaise helps carriers align reserves with actual exposures, reducing reserve volatility and leakage.
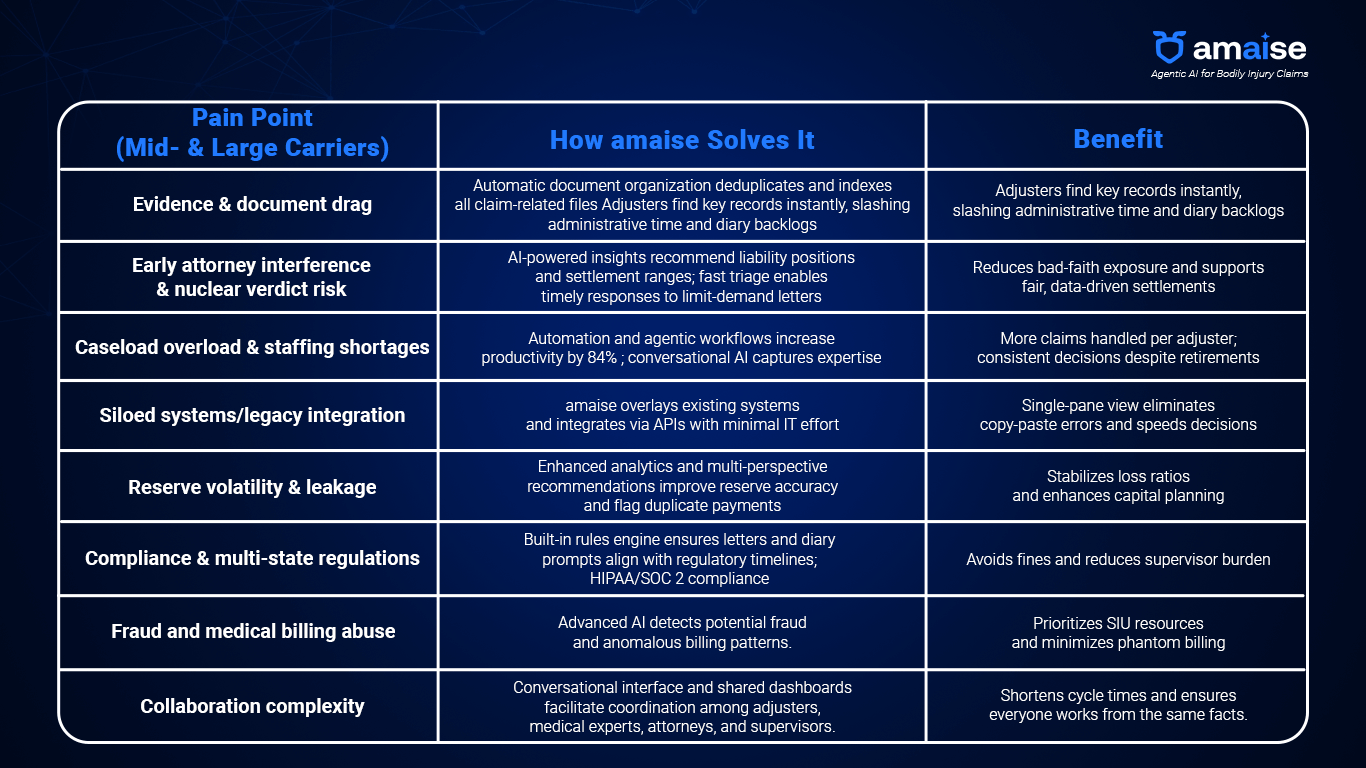
Problem–Solution Map
Why This Matters for Mid‑Size vs. Large Carriers
While many pain points are shared, the scale and resource context differ:
- Mid-size carriers often lack specialized teams. Adjusters may juggle multiple functions, including injury evaluation, litigation, subrogation, and SIU. Technology budgets are lean, making a modular solution like amaise a more attractive option. Automatic document organization and conversational AI reduce administrative burdens, providing analytics typically reserved for larger carriers. Quick pilots and minimal integration effort align with the limited IT resources of mid-size carriers.
- Large carriers grapple with bolt-on legacy systems, multi-jurisdictional compliance, and board-level scrutiny. amaise’s agenticAI layer integrates with existing platforms, aggregates data from disparate sources, and provides early-warning analytics on nuclear-verdict risk and reserve adequacy. The platform’s ability to deliver up to a 13% payout reduction while complying with U.S. regulations appeals to executives focused on combined-ratio improvements and regulatory compliance.
Conclusion
Auto-liability injury claims will only become more complex as medical costs continue to rise and the legal landscape evolves. Average bodily-injury claims already exceed $26,000, and the gap between resources and workloads is widening. Whether you oversee a mid-size regional carrier seeking to empower adjusters with modern tools or manage a top-25 insurer burdened by integration drag and nuclear-verdict exposure,
amaise’s agenticAI Platform offers a path forward. By organizing documents, surfacing actionable insights, enabling conversational collaboration, and delivering quantifiable ROI, amaise transforms the way auto-liability carriers handle injury claims.
Ready to see agentic AI in action? A pilot with just 30-50 claims can reveal how amaise reduces administrative work, improves reserve accuracy, and accelerates settlements. In a market where efficiency and precision make the difference between profit and loss, adopting a specialized AI platform is a necessity.
FAQs
How does amaise integrate with our existing claims system?
amaise overlays your current claims and document-management systems via APIs. A pilot can be launched by uploading 30-50 claims, and full deployment typically requires around 20 person-days.
Does amaise comply with privacy and security regulations?
Yes. amaise is built with complete adherence to U.S. regulations, including HIPAA and SOC 2, ensuring data privacy and secure collaboration across teams.
What evidence is there that AI reduces claim costs?
amaise’s Motor Liability clients have reported up to 84% greater productivity, four-fold improvement in understanding of medical and legal aspects, and a 10% reduction in claim payouts. Leading insurers in Europe achieved a 10% reduction in payouts, and pilots with top U.S. carriers have recorded similar results.